Neurotherapy for Learning Difficulties
Neurotherapy (Neurofeedback) for ADHD and Learning Difficulties

In the neuroscientific community it is widely accepted that ADHD is associated with underlying neurophysiological dysfunctions, mostly involving the frontal lobes. When these dysfunctions are rectified, children with ADHD can process information like children without ADHD, enabling them to develop cognitive skills and coping strategies that are normally acquired during development.
Neuroscientists have known since the mid 1970s that the EEG (brainwaves) of children with ADHD contained an excess of slow (theta) waves and relatively less of the fast (beta) waves. Hence they have a high theta/beta ratio (Janzen, Graap, Stephanson, Marshall, & et al., 1995; Linden, Habib, & Radojevic, 1996; Lubar, 1985; Lubar, 1991; Lubar, 1995; Lubar & Lubar, 1984; Satterfield, Schell, Backs, & Hidaka, 1984; Steinhausen, Romahn, &Gobel, 1984; Tansey, 1991; Watson, Jacobs, & Herder, 1979). Researchers and clinicians have developed techniques to push the brain's Neuroplasticity towards normal to enable children and adults with ADHD to retrain their brainwaves and consequently improve or normalise their behaviours.
What is Neurotherapy?
The neuroscientific community recognises that the abnormal brainwave patterns, shown in QEEG, are associated with a range of cognitive difficulties. Such difficulties include ADHD, depression, anxiety, and psychiatric disorders. Neurotherapy, also called Neurofeedback, is a biofeedback technique that enables individuals to normalise their brain’s electrical activity. Just as physical exercise increases fitness, Neurotherapy is a form of physical exercise for the brain that improves symptoms.

What Does a Neurotherapy Session Involve?
Ordinarily, you cannot influence your brainwave patterns because you lack awareness of them. However, given the opportunity to see your brainwaves on a computer screen, a few thousandths of a second after they occur, you can learn to influence and change them through operant conditioning. Operant conditioning involves reconditioning and retraining the brain on a sub-conscious level. At first, the changes are short-lived, but gradually become more enduring. Through this process, involving continuing feedback, coaching, and practice, Neurotherapy promotes healthier brainwave patterns in most people. As a form of physical exercise for the brain, Neurotherapy enhances cognitive flexibility and control.
What Happens During a Neurotherapy Session?
During typical training, one or two sensors (called ‘electrodes’) are placed on the head, and one on each ear lobe. These sensors are connected to a high-tech EEG device which measures the brain’s electrical activity, much like a physician will listen to someone’s heart from the surface of the chest. The electronic equipment provides real-time (instantaneous) audio and visual feedback about brainwave activity. No electrical currents are put into the brain. The brainwave patterns are recorded, relayed to the computer, and instantly analyzed, before being represented as graphs.
Thus, Neurotherapy is effective for learning disabilities, because it can train the brain to recognise patterns that are unhelpful. Click here to read thecurrent scientific evidence.
Excitingly, even when a problem is biological in nature, Neurotherapy is a viable treatment alternative to medication. It is is also being increasingly used to facilitate peak performance in athletes.
Effectiveness of Neurotherapy For Learning Difficulties
Numerous research papers (Click here for Neurotherapy BIBLIOGRAPHY)(Click here for Neurotherapy BIBLIOGRAPHY), attest to the effectiveness of Neurotherapy. Dr. Jacques Duff, the Director of BNC, wrote a PhD at the Brain Sciences Institute which investigated brain activity in boys with ADHD following Neurotherapy.
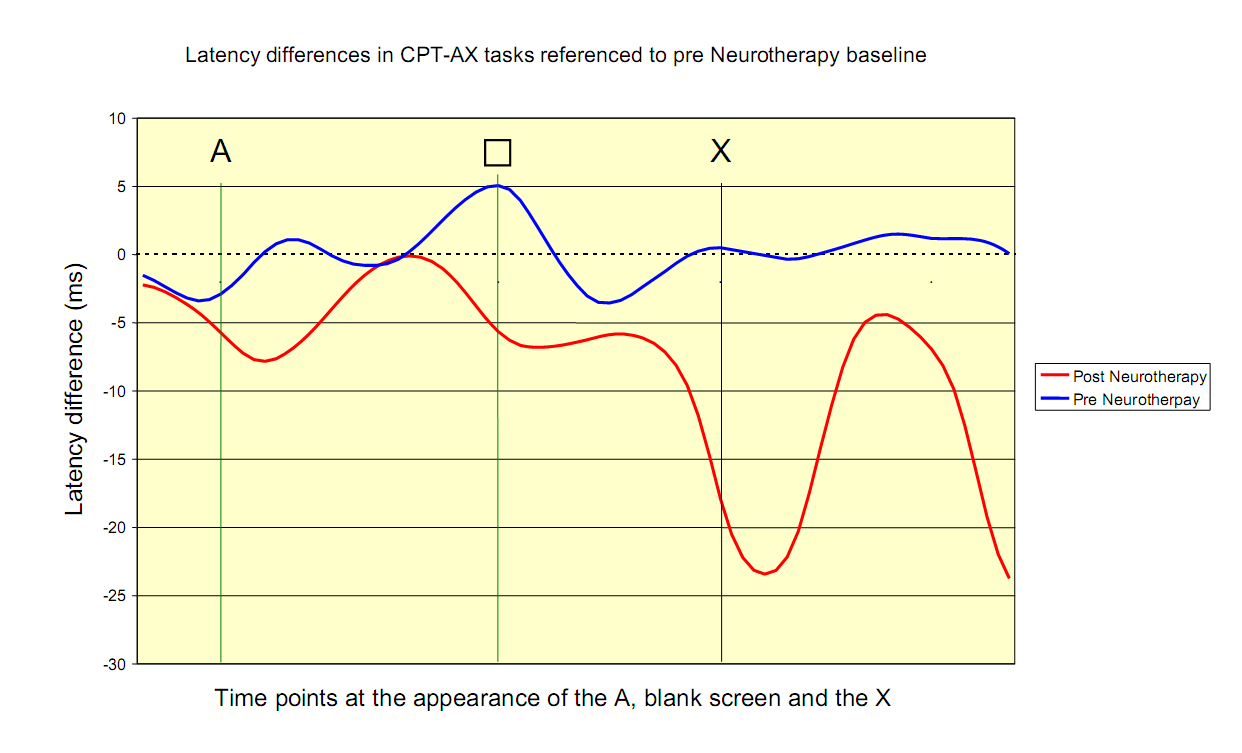
This graph illustrates activation in the right frontal lobe pre- and post-Neurotherapy in the CPT-AX task executed by 17 boys with ADHD. The dashed horizontal line represents a baseline task and is set to zero for both conditions. The computer administered CPT-AX task required the boys to press a button when they saw the letter X, only if the letter before it was an A. The vertical lines represent the time points at which: the letter A is presented (A), the letter A disappears, and the blanking interval commences () and the letter X appears (X). The horizontal blue and red lines represent changes in latency (delay). A reduction in latency is interpreted as increased excitation and a speeding up of brain processes, while an increase in latency can be interpreted as less excitation or a slowing down of processes.
This graph shows that before Neurotherapy there was minimal reduction in latency (no excitation or brain engagement) throughout the CTP-AX task at the right pre-frontal site. On the other hand, following Neurotherapy, there was a large transient reduction in latency on the appearance of the X, suggesting increased excitation and brain involvement. Neurotherapy speeded up the frontal lobe processes necessary for rapidly recognising and processing the target X. Behavioural and TOVA score improvements were seen in all 17 boys with ADHD. All the boys were able to come off stimulant medication. The Neurotherapy treatment for ADHD involves clients viewing a computer screen that displays their brain activity as obtained via EEG sensors on the scalp. Using the computer’s visual and auditory feedback, clients learn to reduce slow (theta) waves and increase fast (beta) waves. The process by which this happens is called operant conditioning and is the mechanism by which we learn most activities in life.
According to the research, after about 20 sessions, the theta/beta ratios start to reduce, and in around 80% of children normalise after 30 to 50 sessions, depending on the severity of their symptoms. As the theta/beta ratio reduces and normalises, hyperactivity and impulsivity reduce or disappear, whilst attention and concentration increase. IQ and cognitive skills also increase.Most of the undesirable behaviours associated with ADHD also reduce or disappear. The brain learns to produce healthier brainwaves, and in doing so acquires the ability to better process information. Once acquired, these abilities are used in every day and therefore are constantly reinforced. Like learning to walk or ride a bike, once learned these skills are retained. There are no negative side effects, and the gains areoften permanent (Lubar, 1991; Tansey, 1993).
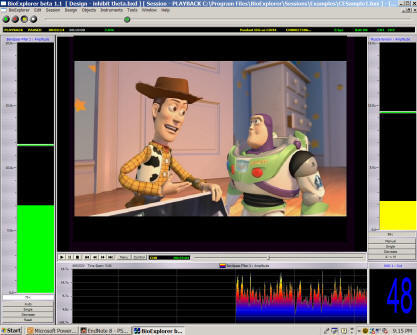
BNC introduced a DVD-based neurofeedback reward system in Australia in 2004. The two bars represent the amplitudes of specific brainwaves. The client uses their brain to control the height of the bars. The DVD plays when the two bars are below the thresholds indicated by the lines. The client is rewarded for controlling his/her brainwave activity. Through a conditioning process, the DVD only plays when the client hit the desired brain frequencies/activity (e.g., the successful suppression of slow brainwave activity). We encourage parents to bring into the clinic, or use at home, a DVD that the child likes, since this will increase their compliance with training.
Improvements in the theta/beta ratios of clients with ADHD following Neurotherapy have been correlate significantly with independent tests as well as parent and teacher reports. After Neurotherapy, scores on Continuous Performance Tasks (such as the TOVA) from thousands of clinics worldwide show improvements on impulsivity, attention, processing speed and distractibility measures.There are also reductions in hyperactivity and impulsivity on behaviour scales, and increases in attention and cognitive skills onindividual achievement and IQtests
Early Neurotherapy Studies

Professor Barry Sterman’s investigation of brainwave patterns of cats during sleep, undertaken in the late 1960s in the EEG Lab at UCLA, discovered that cats could be easily trained through operant conditioning to produce SMR (12-15Hz) brainwave activity for a food reward. In a later study for NASA, the trained cats were found to be highly resistant to chemically induced seizures (from Hydrazine jet fuel). This led Sterman to initiate clinical trials aimed at increasing SMR brainwave activity through Neurotherapy in epileptic individuals. Both seizure rates and EEG abnormalities were significantly reduced in those with epilepsy (Sterman, Macdonald, & Stone, 1974). Sterman went on to publish over a dozen studies on Neurotherapy for seizure disorders and ADHD.
Subsequently, Professor Joel Lubar at Tennessee University published a series of case studies that demonstrated the effectiveness of Neurotherapy SMR training on reducing seizure activity (Lubar and Bahler, 1976). Lubar observed that the seizure patients experienced increased attentiveness, focus and concentration.
This led Lubar to investigate the effects of Neurotherapy on attention deficits and hyperactivity. More studies were to follow thattested the same blind crossover paradigm on larger samples. 75% of the subjects in these studiesshowed increases in SMR which were correlated with a reduction in classroom hyperactivity. The combination of EEG Neurotherapy training with drug treatment resulted in substantial improvements that exceeded the effects of the drugs alone.
In studies where medication was withdrawn, the improvements were maintained with SMR training alone. There was an overall decrease in undesirable behaviours such as disruptive motor activities, self-stimulation, out of seat behaviours and oppositional behaviours. In addition, increases in desirable behaviours were observed, including increased attention span and cooperation. Positive social behaviours also improved, such as self-initiated approaches and sustained interaction with peers and teachers (Shouse& Lubar, 1978; Shouse& Lubar, 1979).
In 1981, Lubar and Deering, a paediatric neurologist, co-published a book which reviewed current clinical research on Neurotherapy, particularly the use of beta/SMR Neurotherapy with theta inhibition to reduce hyperactivity and improve attentiveness (Lubar & Deering, 1981).
To investigate whether Neurotherapy improved school performance, Lubar and Lubar (1984) conducted an experiment with 6 10-19 year old males with ADHD. These siubjects received Neurotherapy for either increasing 12-15 Hz Sensorimotor Rhythm (SMR) or 16-20 Hz beta activity. All children successfully increased their SMR or beta waves, as well as decreased their slow wave EEG and muscle activity (determined by frequency analysis). All subjects made considerable improvementsat school (e.g., higher school grades and scores on the Metropolitan Achievement Test, Peabody, Stanford Achievement test and California Achievement test).
No subjects required hyperactivity medications post- intervention. Thus, if applied comprehensively, Neurotherapy can be highly effective in helping children with attention deficit disorders and difficulties with academic tasks (Lubar & Lubar, 1984). Lubar’s and Lubar’s inaugural study paved the way for Neurotherapy as antherapy for Learning Difficulties.
Neurotherapy And Learning Difficulties
Specific Learning Difficulties may have their basis in minor neurological deficits. Using as few as 8 QEEG variables, learning disabilities can be correctly identified in 75% of cases. With a larger number of indicators, this hit rate goes up to 95%. The best predictor of learning difficulties are excessive 4 to 8 Hz activity in the frontal-temporal locations. Over two years, Neurotherapy aimed at enhancing beta activity successfully remediateslearning difficulties in most children.
In three separate experiments, Lubar et al. assessed the effectiveness of Neurotherapy treatment for 42 children with ADHD and adolescents, aged 8-19 years, on both objective and subjective measures. In the first experiment, the 19 subjects who successfully decreased theta activity showed significant improvement in the Test of Variables of Attention (TOVA). In the second experiment, with 13 subjects, there were significant improvements in the Attention Deficit Disorders Evaluation Scale (ADDES; a parental questionnaire) after Neurotherapy. In thefinal experiment, significant improvements on the Wechsler Intelligence Scale for Children (WISC) wereobserved. All these findings indicate that Neurotherapy is an appropriate and efficacious treatment for children with ADHD and learning difficulties since it promotes cognitive skills and decreases attention deficits (Lubar, Swartwood, Swartwood, & O'Donnell, 1995b).
Lubar et al. also observed that subjectscan learn to decrease the microvolt level of theta over 40 sessions. 12 subjects successfully reduced their microvolt theta levels during Neurotherapy. Despite the training taking place in locations between FZ and PZ, the training effects generalised to most other cortical areas, and the differences were significant. It was illustrated graphically that the 7 subjects who did not learn to decrease their microvolt theta levels showed no improvements at any of the 19 EEG placement sites (Lubar, Swartwood, & Timmerman, 1995a).
If Neurotherapy learning does not take place (i.e., there is no decrease in theta at the training site), then the QEEG shows no changes. Thus, Neurotherapy is directly linked to changes in cortical functioning and is not a placebo effect (Lubar et al., 1995a). Neurotherapy at frontal and central regions may have the power to influence cortical resonant loops, which originate in frontal and central brain regions and are linked to regional and global resonances. This linkage causes other shifts (Lubar, 1997).
In summary, Neurotherapy can normalise the theta/beta ratios shown in the EEG to promote improvements in academic performance, attention deficits, IQ scores, parent and teacher behavioural ratings and schoolwork (grades and achievement test scores; Linden et al., 1996; Lubar, 1991; Lubar, 1995; Lubar et al., 1995b; Lubar & Lubar, 1984; Tansey, 1985).
Comparison of Neurotherapy to Medication
The neurobiological underpinnings of ADHD suggest that the primary focus of treatment should be to address the core issue through decreasing neurophysiological dysregulation. Medication and Neurotherapy come at this from two different angles.Whilst medication attempts to restore neurotransmitter (chemical) imbalance, Neurotherapy challenges the brain todo so through self-regulation.

A study by Rossiter and La Vague compared the effects of Neurotherapy with stimulant medication for reducing ADHD symptoms. A medical treatment program was compared to 20 sessions of Neurotherapy. There were 23 subjects in both groups, matched by age, IQ, gender and diagnosis. The Test of Variables of Attention (TOVA) was administered pre and post treatment. Both groups improved significantly on TOVA measures of inattention, impulsivity, information processing, and variability, and did not differ from each other on TOVA change scores. The results indicate that Neurotherapy is an effective alternative to stimulant medication, with the additional benefit of a lack of side effects.
Lubar and colleagues looked at the QEEGs of 23 individuals with ADHD. Theta/beta ratios, with and without medication (Methylphenidate), were compared.There were no significant effects of the medication on these QEEG ratios at the 19 sites.Thus, the researchers concluded that this medication had very little effect on cortical EEG (Lubar et al., 1995a). In other words, although medication workswhile it is in the system, there is virtually no long-term carryover to a non-dependent state. On the contrary, Neurotherapy works not only during the training, but has a carryover effect that can last a lifetime (Lubar, 1997).
