ADHD Treatments & Therapies
The following are the options for ADHD treatments:
- Neurotherapy
- Diet & Nutrition
- Medication
- Counselling
- Cognitive Behavioural Therapy
- Family Therapy
We will discuss the above methods in detail below.
Neurotherapy for ADHD Treatment
.jpg)
Since the early 1970s, research and clinical practice in Neuroscience and Psychophysiology has shown that Neurotherapy can encourage brain plasticity and promote the normalisation of the brain patterns that underlie ADHD behaviours. Neurotherapy has been shown to be as effective as stimulant medication for ADHD.
There are currently more than 20,000 clinicians worldwide using Neurotherapy for permanent remediation of ~80% of ADHD cases, and other mental disorders, without the use of drugs. However, the great work of psychologists, psychiatrists, neurologists, and medical practitioners using Neurotherapy goes largely unrecognised. In part, this is due to lack of interest from the medical and pharmaceutical industries.
Neurotherapy is computer-based brain retraining that promotes more normal patterns of electrical activity. It has been shown to be an effective treatment for around 80% of children with ADHD and Learning Difficulties.
In the 1970s, Neurotherapy was developed at the UCLA Medical School EEG Laboratory by Professor Barry Sterman as a therapy for childhood epilepsy. It was further developed by Professor Joel Lubar of Tennessee University as a treatment for ADHD and Learning Difficulties. To date, there are over 300 studies that show Neurotherapy to be an effective treatment for ADHD and learning difficulties. Therapy effects appear to last for years, some for life.
Neurotherapy Research Findings
In the January 2000 issue of ‘EEG and Clinical Electroencephalography’, a journal from the EEG and Clinical Neuroscience Society, was a focused review of Neurotherapy. Professor Frank H. Duffy, M.D., a paediatric neurologist at Harvard Medical School, stated that Neurotherapy should play a major therapeutic role. In his opinion ‘If any medication had shown such a wide range of benefits with no adverse side-effects it would be widely used and accepted.’
PET, fMRI, SPECT, LORETA, and other neuro-imaging studies have revealed QEEG patterns specific to children with ADHD. EEG shows that children with ADHD have slower wave power in Delta (1-4 Hz) or Theta (4-7 Hz) and/or Alpha (8-13 Hz) and reduced fast wave Beta (16-30 Hz) activity, when compared to age-matched controls. Approximately 10% of these children have abnormally high Beta activity, potentially due to environmental toxins or a mutated COMT gene.
During Neurotherapy, real-time QEEG is displayed on a computer in the form of a game, and the patient is given contingent audio-visual rewards for producing faster brainwaves. There is significant evidence which suggests that most children with ADHD can learn to produce brainwave patterns with more normal theta/beta ratios.
Improvements following Neurotherapy in the theta/beta ratios of patients with ADHD correlate with many empirical and subjective measures. These theta/beta ratios are correlated with improvements in ‘impulsivity’, ‘attention’, ‘response time’ and ‘variability of response time’ scores on the Test of Variables of Attention (TOVA) and Continuous Performance Tasks. In addition, we see reductions in hyperactivity and impulsivity on behaviour scales, increases in attention and cognitive skills in Individual Achievement Tests scores, and increases in IQ scores.
Neurotherapy is effective in over 80% of cases in significantly reducing ADHD symptoms, and the effects appear permanent. In randomised controlled trials, participants with ADHD on psycho-stimulant medication at the start of the study can significantly reduce their dose, or come off it entirely, by the end of their Neurotherapy training.
Many researchers, scientists, and clinicians are dissapointed that Neurotherapy is not used widely. Pharmaceutical companies have little interest in funding this research in clinical settings.
Studies Comparing Neurotherapy to Ritalin
The neurobiological underpinnings of ADHD suggest that the primary focus of therapy should be to address the core issue i.e., remedying neurological dysregulation. While medication chemically modulates neurotransmitter activity, stimulating changes in the brain’s electrical activity, Neurotherapy challenges the brain to achieve self-regulation by promoting brain plasticity. Methylphenidate and other stimulants, used to enhance attention, only produce state-dependent effects. Whilst the medication works while it is in the person's system, there is virtually no long-term carryover to the non-dependent state. Instead, Neurotherapy works not only during training, but has a carryover effect that can last a lifetime (Lubar, 1997).
Rossiter and La Vague compare the effects of Neurotherapy with that of stimulant medication in reducing ADHD symptomatology. A medical treatment program, administered over 20 sessions, was compared to the effects of Neurotherapy. The Neurotherapy group (N=23) was matched with a stimulant group (N=23) in age, IQ, gender, and diagnosis. The TOVA was administered pre and post treatment. Both groups showed significant improvements on TOVA measures of inattention, impulsivity, information processing, and variability, and TOVA change scores did not differ. Thus, Rossiter concluded that Neurotherapy is as effective as stimulant medication and may serve as a promising alternative when medication is ineffective, produces adverse side effects, or is not taken compliantly.
To compare the effectiveness of Neurotherapy to stimulant medication, 22 children from a social-paediatric hospital (8 to 12 years of age), with a primary diagnosis of ADHD, were assigned to an experimental Neurotherapy group. The group received thirty 45-minutes sessions of Neurotherapy to enhance SMR and/or beta activity, and suppress theta activity, over a period of 10 weeks. The control group consisted of 11 children, who were matched in age and sex, but were medicated with Methylphenidate (Ritalin). No other psychosocial therapies or medication was administered to either group. The test battery consisted of an IQ test (HAWIK-R), TOVA, paper-pencil-test (d2) and IOWA Conners Behaviour. These measures were administered pre- and post-treatment to both groups. Both groups (medicated and undergoing Neurotherapy) showed significant improvements in attention and concentration across both objective and subjective measures. Performance IQ scores also improved significantly in both groups. However, whilst the results indicate that Ritalin and Neurotherapy had comparable effectiveness, the gains from Neurotherapy are expected to be permanent, while the gains in the medicated group are undoubtedly dependant on the daily use of the Ritalin [1].
One hundred children (age 6-19) diagnosed with ADHD (inattentive or combined types), participated in a one-year, multimodal, outpatient program that included prescription Ritalin, parent counselling, and academic school support. Fifty-one of these children also received Neurotherapy. Pre- and Post-treatment assessments were conducted to both groups on and off stimulants. Significant improvements were observed on the TOVA and the Attention Deficit Disorders Evaluation Scale [2] when participants were tested while on Ritalin. However, only those who had received Neurotherapy sustained these gains when tested off Ritalin. Only those who had did Neurotherapy had reductions in theta/beta power ratio and these changes were statistically significant. The ADDES behavioural measures also showed that parenting style moderated the expression of behavioural symptoms only at home, not at school [3].
Fuchs and colleagues compare the effects of a 3-month Neurotherapy program which rewarded SMR (12-15 Hz) and beta activity (15-18 Hz) to Methylphenidate (Ritalin) treatment. Thirty-four of these children (age 8-12 years) with ADHD were assigned to a Neurotherapy group, and 12 children to a methylphenidate group according to their parents' preferences. Both the Neurotherapy and methylphenidate were associated with improvements on all scales of the TOVA, and speed and accuracy results for the Attention Endurance Test. ADHD behaviours were significantly reduced in both groups — shown by the IOWA Conners Behaviour Rating Scale, and teacher/parent ratings. Thus, it was concluded that Neurotherapy is as effective at improving ADHD behaviours as stimulant medication [4].
Study Replication
Rossiter replicates an earlier study [5] with a larger sample of ADHD patients of a wider age range. He also undertook more advanced statistical analysis techniques and collected more comprehensive behavioural data from the Neurotherapy group. Thirty-one patients who chose methylphenidate treatment were matched with 31 patients who chose Neurotherapy. Of the Neurotherapy patients, 14 received training in the clinic, while the remaining 17 received training at home. Kazdin describes the study design an ‘effectiveness research’ whereby patients chose assignment to either the Neurotherapy group or the Methylphenidate (active treatment) control group [6]. The Methylphenidate dose was titrated based on TOVA results. Both groups showed significant improvements on TOVA measures (84% compared to baseline).
There were large effect sizes for Neurotherapy (1.01-1.71) and Medication (0.80-1.80), and individual TOVA scores also improved (Neurotherapy: 55%, Methylphenidate: 56%). Post-intervention averages for both groups fell within a normal range of functioning. Large effect sizes showed improvements in behaviours across groups. The improvements in the Neurotherapy group were equivalent to those seen in the medicated group. Confidence intervals and non-equivalence null hypothesis testing confirmed that the Neurotherapy program produced patient outcomes equivalent to those obtained when taking stimulant drugs [7].
The results of this study [7], the reanalysis of data from Rossiter and La Vaque (1995), and other studies comparing Neurotherapy to Medication [1, 3, 4] support the view that Neurotherapy produces patient outcomes that are equivalent to, or non-inferior to, those obtained with Methylphenidate. However, Rossiter quite rightly pointed out the effectiveness research design limits the conclusions that can be drawn. Effectiveness studies are typically conducted in clinical settings and utilise patients who often have co-morbidities, meaning that their individual protocols were tailored based on their presenting symptoms and baseline EEG data. Compromises such as this sometimes need to be made in research, since it is good ethical practice to give participants autonomy in decision-making. These deviations are acceptable for an effectiveness study but would be considered flaws in an efficacy study. Despite this, the studies demonstrate that Neurotherapy is clinically effective. Yet they shed little light on the various elements contributing to positive outcomes (e.g., the nature of the treatment, patient expectations, therapist characteristics, and the role of placebo effects.) [7]
Effectiveness versus Efficacy Studies
As others argue [6], while efficacy studies place emphasis on internal validity, effectiveness studies place greater emphasis on external validity, i.e., real life effects. Effectiveness studies evaluate therapies as they are conducted in clinical practice, whilst efficacy studies cannot. Therefore, an effectiveness research design is necessary to demonstrate applicability in real life since they sample a broad spectrum of patients (not only clinical/hospital populations) (Clarke, 1995). However, the issue remains that we cannot solely attribute improvements in ADHD to the effects of Neurotherapy, since the influence of nonspecific factors cannot be ruled out. However, the results are promising given that studies [1, 3, 4] independently obtained similar results with different clinicians, settings, patient populations, and treatment protocols [7].
1. Fuchs, T., Attention and Neurofeedback. 1998.
2. Adesman, A.R., The Attention Deficit Disorders Evaluation Scale. Journal of Developmental and Behavioral Pediatrics, 1991. 12(1): p. 65-66.
3. Monastra, V.J., D.M. Monastra, and S. George, The effects of stimulant therapy, EEG biofeedback, and parenting style on the primary symptoms of attention-deficit/hyperactivity disorder. Appl Psychophysiol Biofeedback, 2002. 27(4): p. 231-49.
4. Fuchs, T., et al., Neurofeedback treatment for attention-deficit/hyperactivity disorder in children: a comparison with methylphenidate. Appl Psychophysiol Biofeedback, 2003. 28(1): p. 1-12.
5. Rossiter, T.R. and T.J. La Vaque, A comparison of EEG biofeedback and psychostimulants in treating attention deficit/hyperactivity disorders. Journal of Neurotherapy, 1995. 1(1): p. 48-59.
6. Kazdin, A.E. and M.K. Nock, Delineating mechanisms of change in child and adolescent therapy: methodological issues and research recommendations. J Child Psychol Psychiatry, 2003. 44(8): p. 1116-29.
7. Rossiter, T., The effectiveness of neurofeedback and stimulant drugs in treating AD/HD: part II. Replication. Appl Psychophysiol Biofeedback, 2004. 29(4): p. 233-43.
Dietary Changes and Nutritional Supplementation
‘Diet’ is the term given to what you eat, whilst ‘nutrition’ is what you absorb from your diet. Food is processed by digestive enzymes and broken down into nutrients by beneficial bacteria in the small and large intestines. Abnormal bacterial profiles are characterised by a significant reduction in beneficial bacteria, and an increase in other bacteria counts. In these cases, the breakdown of food is less optimal and nutrient uptake may be inadequate.
Additives, artificial colourings, flavourings, and other chemicals (including prescribed medications such as antibiotics) may interfere with the delicate balance of beneficial bacteria in our gut. The antibiotics we find in foods are also detrimental to healthy gut bacteria. Additionally, modern agricultural methods and food processing systems, which were unavailable to our evolutionary ancestors, have significantly reduced the availability of nutrients in our food.
The ‘Medline’ medical database contains numerous references to studies highlighting the benefits of vitamins and nutrients for a range of mental health disorders.
The Critical Importance of Omega 3 Essential Fatty Acid (EFA)
Of all nutrient deficits, none appear to have such widespread ill-effects as deficiencies in Omega 3 EFAs derived from fish. Most bookstores have at least a dozen books on the benefits of fish or fish-oil consumption. All modern diseases have been linked to deficits in fish-derived Omega 3 fatty acid. To name a few: ADHD, Learning difficulties, depression, anxiety, bipolar disorder, schizophrenia, diabetes, cancer, cardiovascular disease, and Alzheimer’s Disease. For a comprehensive review of this literature, we recommend the book titled ‘The Omega 3 Connection,’ by Professor A. Stoll, the Head of Psychiatric Pharmacology at Harvard Medical.
Studies and reports by the World Health Organisation, the US. National Institute of Health, and Australia’s NHMRC, recommend that we should consume a ratio of Omega 6 to Omega 3 of around 2:1. Communities who consume this ratio have a very low incidence of most modern diseases. However, in our modern, predominantly Western diet, we consume a ratio of Omega 6 to Omega 3 around 20:1 to 40:1.
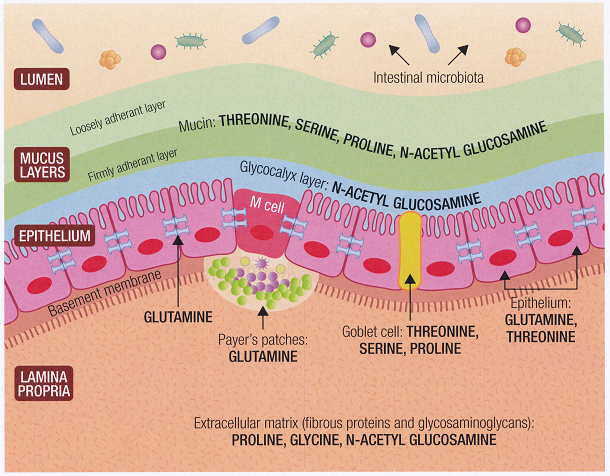
Every cell in the body has a lipid (Essential Fatty Acid) membrane which acts to protect the cell from external substances. Omega 3 fatty acids play a crucial role in this protection. A lack of Omega 3 EFAs makes every cell in the body vulnerable. The most affected areas are the brain and the gut wall, and in children the ear and mucous membranes of the nose, throat, and lungs.
Omega 3 EFAs and Brain Function

The brain consists of 70% lipid, and 40% of it is made up of Omega 3 EFAs (the kind we get from fish). There are more than 8000 studies on Essential Fatty Acids in the scientific literature. Many are animal studies that demonstrate that deficiencies of long chain Omega 3 EFAs are associated with serious brain and systemic dysfunctions. Omega 3 EFAs are essential for brain function. Deficits are associated with psychiatric disorders including ADHD and Learning Difficulties.
Omega 3 EFAs and Gut function in ADHD
The gut cell wall (epithelium) is exposed to billions of organisms and toxins daily. The importance of the lipid membrane is to protect each cell. If the lipid membrane is faulty (e.g., there are deficits in Omega 3 fatty acids) protection fails and unfriendly organisms, irritants, and toxins irritate the gut wall. This can lead to a leaky gut and food sensitivities.
Of course, it is not that simple since there are hundreds of nutrient interactions and systems at play. However, the lipid membrane hypothesis suggests that in genetically susceptible people, Omega 3 deficiencies trigger a chain of events that can lead to many modern diseases. See Harvard Professor Andrew Stoll's book ‘The Omega 3 Connection’ for more details.
Irritants and ADHD
In a double-blind placebo-controlled crossover study at the Royal Prince Alfred Hospital, children (N=27) on an elimination diet (which excluded food additives, natural salicylates, amines, and glutamates) were compared to those challenged with calcium propionate (preservative 282) or given a placebo in their daily bread. There were clinically significant improvements in ADHD behaviours for those on the elimination diet.
There was a significant difference in the proportion of children whose behaviours worsened with the challenge compared to placebo. Dengate and Ruben, who ran the study, inferred that for children sensitive to salycilates, amines, glutamates, and food additives, their irritability, restlessness, inattention, and sleep disturbance was caused by the common preservative.
Additive 282 exacerbates problematic behaviours in children, and this study also highlights that some children benefit from a diet that excludes substances including amines. Removing these irritants in the gut helps reduce problematic, and when reintroduced the behaviours return.
Repairing the GUT wall
In addition to removing irritants from the diet, the gut wall needs to be repaired using specific nutrients, including Omega 3 EFAs and specific amino acids. The gut’s bacterial balance should be restored, through a reduction in sugar, refined carbohydrates, wheat, and cereal grains – all of which can be replaced with legumes and vegetables. Transitioning to this diet can take several months, but in our experience most children thrive on this diet, with parents and teachers reporting behavioural improvements. We see best results when children on this diet also take part in Neurotherapy, to address abnormal brainwave patterns, and CBT, to help them better adapt to their environment and promote functional behaviours.
Food allergies and abnormally high levels of naturally occurring bowel bacteria can increase amine production in the gut. Recent evidence suggests that these trace amines trigger the brain’s neurotransmitter receptors, resulting in mental fog, fatigue, and medication-resistant depression. This may be why ~ 40% or people respond to anti-depressants and 30% to placebo.
Omega 3 supplements are an important component of nutritional supplementation at BNC as part of our ADHD therapies, Learning Difficulties, and other developmental disorders.
Amines, depression, and impaired mental function in ADHD
Amines are naturally occurring substances in food, which the body can tolerate in small amounts. However, in larger quantities they can cause serious brain disturbances, triggering depression and reducing mental alertness. Recent studies examining amine receptors in the brains of mammals, including humans, suggest that increased dietary amines along with increased amine production from the overgrowth of certain gut bacteria, causes depression and a ‘scrambling’ of brain messages, resulting in a foggy mind and poor concentration.
Medication for ADHD
For decades, stimulant medications have been used to treat the symptoms of ADHD. Two of these medications are methylphenidate (Ritalin) and Dexamphetamine. It is proven that they are effective in reducing symptoms in 40-60% of children with ADHD. However, most prescription psychiatric drugs have the potential for adverse side effects.

Ritalin, and other stimulants, spark controversy. The potential for side effects should be weighed against the benefits before these drugs are prescribed. Children on these medications may lose weight, appetite, and grow more slowly. Others have problems falling asleep.
It is under discussion whether stimulant medications aggravate TICS and other Tourette’s symptoms. After noting a child’s height, weight, and overall development, doctors often conclude that the benefits of medication outweigh the potential side effects, and that side effects can be managed by a reduction in dosage. However, that is not true for all children. Thus, parents should educate themselves on both sides of the debate before making their decision.
Another question is whether Ritalin and other stimulants are prescribed unnecessarily for too many children. Keeping in mind that many things, such as diet, poor nutrition, anxiety, depression, allergies, seizures, and problems at home and/or school make children overactive, impulsive, or inattentive, it is possible the medication is not the full answer. Critics of medication argue that many children without ADHD are medicated to control undesirable behaviours, when dietary changes, nutrient supplements, Neurotherapy and counselling should be the first option.
Unfortunately, for some children, being scolded or punished is the most attention that they get. They have little opportunity to build a sense of worth and competence. Whilst medication can help control behavioural problems that lead to family turmoil, there are often aspects of the problem that medication cannot improve. ADHD is a disorder that has broad emotional and academic repercussions. In the scientific literature there is no evidence that stimulant medication promotes long-term improvements in academic or cognitive areas.
Counselling for Children with ADHD

If children are hyperactive, they are often told that they are naughty and punished for being disruptive. If they are disorganised, and unfocused in tasks, they may be called lazy. If they impulsively grab toys, interrupt conversations, or push their classmates, they lose friends. If they have a related conduct disorder, they may get into trouble at school, or even with the law. People with ADHD often experience the daily frustrations of living with disorder, as well as the fear that others think that they are strange, abnormal, or stupid.
These cycles of frustration, blame, and anger, persist for so long that breaking them is hard. Children and their parents need help to develop healthy techniques for managing these cycles of cognition, affect, and behaviour. A developmental psychologist who counsels the child and/or their family, can help them develop new skills, attitudes, and ways of relating to each other.
In individual counselling sessions, a psychologist helps people with ADHD feel better about themselves. People can learn to recognise that having a disability does not reflect who they are as a person. A psychologist helps people with ADHD identify and build on their strengths, cope with daily problems, control their attention and aggression. In counselling, people learn that they are not alone in their frustrations and that help is available.
Sometimes only the person with ADHD requires counselling. Yet in many cases, all family members need support due to the functional impact of ADHD. A psychologist can help the family find better ways to promote change. If the child is young, most of the psychologist’s work is with the parents, teaching them techniques for coping and improving their child’s behaviour.
Cognitive Behavioural Therapy (CBT) in ADHD
CBT refers to a group of therapies that aim to reduce a person’s dysfunctional cognitions and behaviours by helping them identify and alter their underlying thinking patterns. In other words, you learn to replace maladaptive behaviours with adaptive ones. The basic concept of CBT is that behavioural change has a flow-on effect to other areas of functioning. CBT is a therapeutic intervention which promotes new replacement behaviours, identifies unhelpful thinking patterns, and teaches healthy self-talk. However, there is no evidence that CBT is effective at bringing about permanent change in the core symptoms of ADHD. However, CBT when combined with nutritional supplementation and Neurotherapy, can promote psychosocial skills, minimise low self-esteem, and the ADHD’s biological underpinnings.
ADHD Therapies for Family
Family therapy can help families improve their communication skills. Family therapy involves training in communication, interpersonal relations, conflict resolution skills, boundary setting, and healthy discipline.
Not all families require counselling, and those who do may need help only in some areas.
Summary of Modalities for ADHD Treatments
- Stimulant medication and antidepressants are recommended in the short term.
- Antibiotics may be used for bacterial infections together with (or followed by) probiotics to replace beneficial gut bacteria.
- Neurotherapy addresses abnormal brainwave patterns and promotes functionality.
- Dietary interventions are highly recommended, along with nutritional supplementation.
- Family counselling, CBT and Intensive Behavioural Modification are all advisable.



